Special Report: An Overview of Coronavirus by Dr. Jonathan Kaplan

Wash your hands, wipe down surfaces, don’t touch your face, and practice social distancing. If nothing else, that’s what you should take away from this coronavirus overview. But keep reading to learn important details about this epidemic. Such as, how we can make it end with less collateral damage? How does it compare to a typical annual flu season? This coronavirus overview is based on science, epidemiology, and facts. No “fake” news and no political or socioeconomic commentary (until the very end).
Coronavirus Overview: The Basics
This newly discovered coronavirus is “SARS-CoV-2” (Severe Acute Respiratory Syndrome – Corona Virus – version 2 (the first version discovered in February 2002 in China)) and the disease it causes is COVID-19 (COrona VIrus Disease discovered in 2019).
While the first case or patient 0 is not known, it is believed the virus was passed from animal to human in a seafood and live animal market in Wuhan, China according to the CDC. COVID-19, like many other coronaviruses, spread from bats.
Keep in mind that not all coronaviruses are so life threatening. Some coronaviruses are responsible for the common cold. But COVID-19 is a new, or novel, coronavirus that is potentially life-threatening and for which no one has immunity. Until of course, they contract the disease and recover, rather than succumb to it.
How It Is Spread
Persons infected with COVID-19 become symptomatic approximately two to 14 days after contracting the virus. This is why testing of the disease prior to symptom onset is important. The hope is that if someone tests positive before they experience symptoms, they will self-quarantine and non unwittingly infect others.
Unfortunately, the potential for an asymptomatic person spreading the disease without knowing they have it, and therefore not practicing social distancing, is very real. The CDC has said that asymptomatic carriers are not the main driver of disease, which may be true. But asymptomatic transmission may be a bigger risk than initially understood.
For those that are symptomatic, symptoms include fever, sneezing and coughing initially. Thereafter, the disease can progress to severe respiratory failure, especially in elderly adults. Those with chonic illnesses, such as heart disease or diabetes are also at greater risk. Keep in mind, over 80 percent of cases are mild and do not require hospitalization. Currently, based on a recent compilation of data from the New England Journal of Medicine, the risk of death is one percent, which is 10-times greater than the risk of death from the “typical” annual flu, which is < 0.1 percent.
The virus is present in secretions of the nose and mouth. The virus spreads via coughing or sneezing directly onto another person. And those virus-infested droplets can subsequently land on a surface that someone can touch, and then touch their face, leading to infection. The route of transmission is the basis for the now well known recommendations to wash your hands for 20 seconds, avoid touching your face, and social distancing of six feet.
Face masks of the N-95 type are recommended for sick individuals. These masks fit tightly to the face, minimizing the risk of spread. However, it would be more optimal for sick individuals to remain at home. There is no benefit to healthy adults wearing masks of any type.
The Spread of COVID-19
According to this article in the New England Journal of Medicine, and an excellent visual representation in the Washington Post, COVID-19 has an estimated reproduction number (R0) of 2.2. The higher the R0, the more infectious, or the faster the spread of the disease. In the case of COVID-19, the R0 means each infected person will give the infection to an additional two persons. For comparison, measles, which was mostly eradicated by a vaccine, has a higher R0 of between 12 and 18, with each person spreading the disease to 12 to 18 other individuals!
Keep in mind that how contagious a disease is differs completely from how deadly it is. For example, the ebola virus has a R0 of less than 2 (less contagious). But it kills half the people that become infected.
Aside from individually doing our part of social distancing, what can society as a whole do? This Washington Post article explains, in visual simulations, how a fictitious disease spreads. Without any intervention, COVID-19 could have an exponential rate of spread, doubling the number of cases every three days. This would result in the infection of 100 million cases in the US by May! But again, this is without any intervention.
What Stops the Spread of COVID-19?
So what interventions does the CDC recommend? The goal of any intervention is to slow the number of people that get the disease and also minimize the number of people that have it at any one time, resulting in a growing number of recovering patients who can no longer spread the disease.
A forced quarantine in theory works. If there is a well-defined area of people that have the disease and the authorities don’t let them out of that area, then they can’t spread it farther (i.e., a cruise ship). Unfortunately, as mentioned above, some asymptomatic people will leave the defined area 1.) before they know they’re sick and 2.) before it’s clear there is an epidemic in the first place and thus, before a quarantine has been established.
Another option is the banning of public gatherings and the individual’s choice to avoid any gatherings not already banned. With fewer people around, the virus is more limited in its ability to spread to others. This includes the cessation of March Madness and the NBA season. Possibly the delay of the baseball season, the cancellation of the Olympics, and school closures. Therefore, social distancing, on a community-wide level, or moreover, on a nationwide level is the best way to slow the spread.
Cautious Optimism in Hong Kong, Taiwan, and Singapore
Not only do these techniques work in theory, they’re shown to work in the midst of this current crisis. Hong Kong, Taiwan, and Singapore—all with very low rates of infection despite being in such close proximity to the epicenter of COVID-19—show the benefits of banning travel from areas of infection and reducing public gatherings. If there is a linear rate of infections, the United States’ recent efforts in banning public gatherings has resulted in a confirmed infection rate (0.00085%) better than Singapore (0.0035%) and Hong Kong (0.0019) but trailing Taiwan’s infection rate of 0.00025% as of March 15, 2020.
The irony of instituting these behavioral modifications on society as a whole is that if it reduces the number of infections over the course of the epidemic in the US, everyone who said we as a nation were overreacting will say, “I told you it wasn’t going to be that bad!”
Flattening the curve
You may have seen this recent “flatten the curve” meme across the internet.
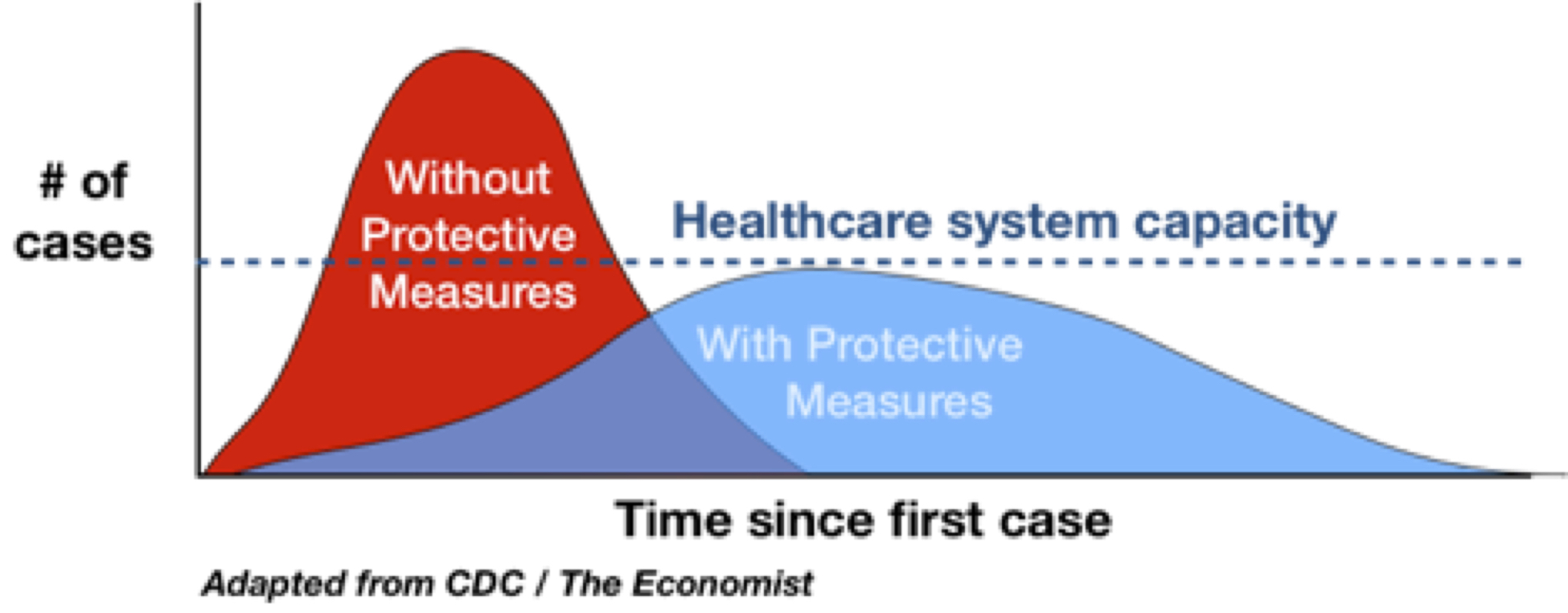
Important to remember that #Covid-19 epidemic control measures may only delay cases, not prevent. However, this helps limit surge and gives hospitals time to prepare and manage. It’s the difference between finding an ICU bed & ventilator or being treated in the parking lot tent. pic.twitter.com/VOyfBcLMus
— Drew A. Harris, DPM, MPH (@drewaharris) February 28, 2020
This graphic was first created in 2007 as part of a CDC article regarding a future pandemic. The graphic describes how the use of simple interventions like hand washing and keeping kids home from school can slow a pandemic. By slowing the spread of the disease and flattening the curve, the healthcare system can acclimate to the needs of the public and ramp up their response. This will allow sick individuals to get the care they need, i.e., ICU beds and ventilators. This, in contrast to the situation in Italy where some are left to die because there are no ventilators available, since so many people got so sick, so fast.
How This Coronavirus Compares to Other Respiratory Syndromes and the Annual Flu
COVID-19 shares approximately 80 percent of the genetic material of the coronavirus that caused SARS-CoV, the virus that emerged in 2002-2003 in Guangdong, China. While they are similar, they have very different infection and mortality rates. SARS infected over 8,000 people, killing about 800, whereas COVID-19 has infected 142,539 and killed 5,392 as of March 15, 2020. In other words, SARS reproductive capacity to infect others (R0) was low when compared to COVID-19, but so far, SARS has a higher mortality rate (more patients died). The reason is not quite clear but has to do with the ability of SARS to infect the deeper portions of the lung, causing pneumonia. Whereas COVID-19 is often more restricted to the mucus membranes of the nose and mouth, typically causing flu-like symptoms.
And while it’s easy to focus all of our attention on COVID-19, don’t forget the severity of the annual flu. The flu/influenza virus, despite having a vaccine, was the cause of 34 million cases of flu this year in the US! 350,000 of those cases resulted in hospitalizations and 20,000 deaths (<0.1%). Certainly most flu cases are milder and the mortality rate is lower than COVID-19. But these numbers speak to the importance of vaccination, washing hands and social distancing as a general rule going forward.
Where Do We Go From Here?
Once tests are more readily available in your area, it’s worth getting one for COVID-19. By knowing if you’re asymptomatically positive, you can do your part to self-quarantine and reduce the spread. (At the time of this writing, due to low supplies, testing is only recommended for healthcare workers in close contact with infected patients, hospitalized patients and those with symptoms of fever and cough with underlying medical problems).
Vaccination can be a touchy subject for many. But can a stronger case be made to vaccinate for the annual flu virus, and for COVID-19 once available?
While doing what we can to stay healthy, we should also adjust our lifestyle in a way that remains fulfilling. If possible, work from home. We have email and videoconferencing now, options not available during the 1918 flu epidemic. Worried about going to a restaurant? Continue to order food from your favorite restaurant via food delivery apps. A doctor’s visit? Many doctors offer televisits for checkups and consults.
In other words, we should heed the advice of the CDC, but keep our economy moving along as best as possible. Because my fear is that after we weather the storm of COVID-19, we’ll enter an economic storm of a different sort. Our collective economic health goes hand in hand with our goal of being physically and mentally healthy.
Stay safe and stay healthy!
Dr. Kaplan also shared advice on how technology can help physicians stay in touch with patients for consultations and any needed follow-up appointments in our special combined episode of MATV and DermWire TV. Watch the epsidode here. And learn more about the technology Dr. Kaplan uses by visiting www.pacificheightsplasticsurgery.com/pricing.
