Advances in the Treatment of Reticular Erythematous Mucinosis
Reticular erythematous mucinosis (REM) is a rare and chronic form of plaque-like mucinosis with unknown pathogenesis and etiology characterized by pink or red papules in a net-like pattern on the chest or back (Figure 1).1 REM is most common in young and middle-aged females.
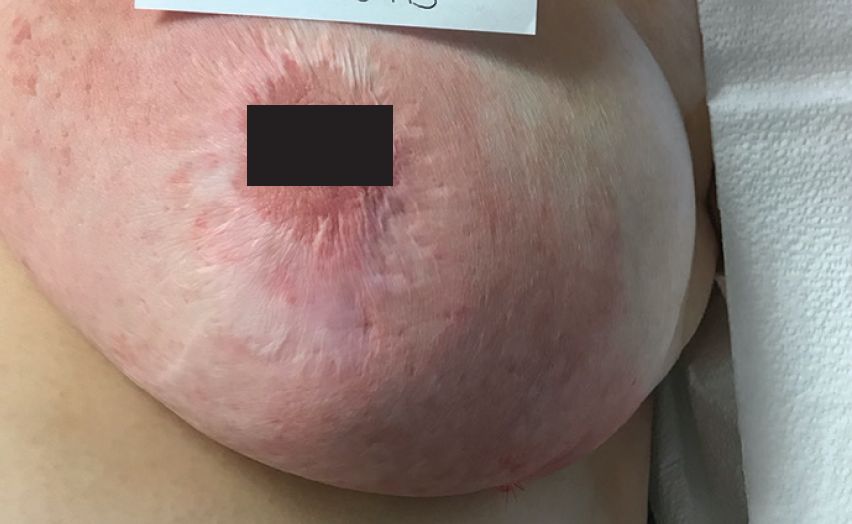
Figure 1. Erythematous indurated patch with satellite papules on the left breast.
REM has been found to be associated with altered states of immune function, specifically circulating immune complexes such as idiopathic thrombocytopenic purpura, as well as diabetes mellitus, thyroid disease, and neoplasia.2,3 Additionally, exposure to sunlight has been shown to increase severity; however, some cases have improved with sunlight.2,3
Histopathologically, REM is characterized as mucinous deposits between bundles of collagen in the dermis.4
Case Study: A 56-year-old woman with REM
A 56-year-old woman with a history of hypertension, gastroesophageal reflux disease (GERD), superficial blood clots, osteoarthritis, hypothyroidism, and obesity was hospitalized multiple times requiring care in the intensive care unit due to progressive eruptions of a red indurated patch and papules on the left breast (Figure 1). A biopsy was performed and histopathology showed focal parakeratosis, mild acanthosis, and focal basal vacuolar changes (Figure 2).
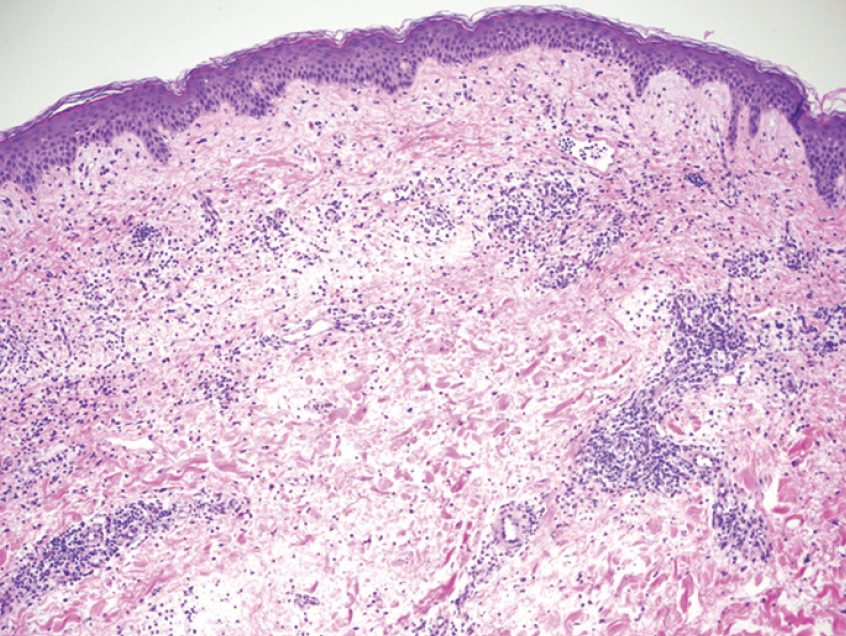
Figure 2. Focal parakeratosis, mild acanthosis, focal basal vacuolar changes (H&E, original magnification x 100).
Additionally, histopathology showed superficial and deep, perivascular lymphoplasmacytic infiltrates with rare eosinophils in the dermis (Figures 3 and 4). A colloidal iron stain revealed slightly increased dermal mucin content (Figure 5). PAS, gram, and Fite stains were negative for microorganisms. A diagnosis of reticular erythematous mucinosis was made.
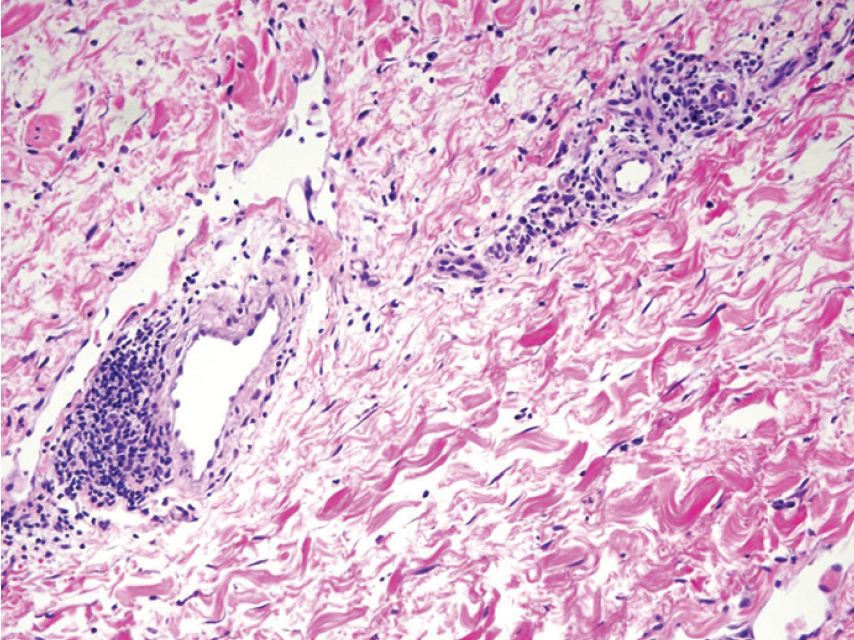
Figure 3. Superficial and deep, perivascular lymphoplasmacytic infiltrates with rare eosinophils (H&E, original magnification x 200).
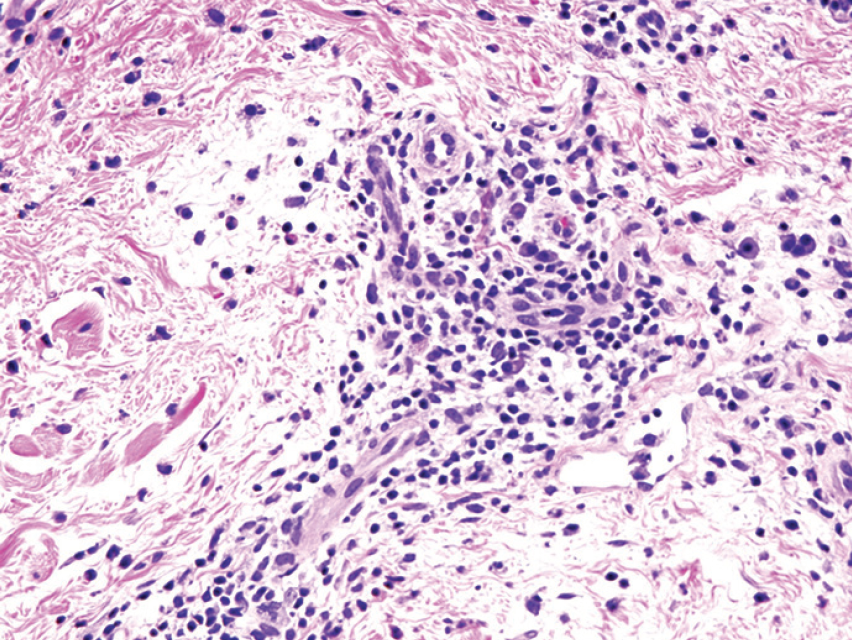
Figure 4. Superficial and deep, perivascular lymphoplasmacytic infiltrates with rare eosinophils. (H&E, original magnification x 400).

Figure 5. Colloidal Iron (mucin) stain (original magnification x 100).
Though ultraviolet A1 light (UVA1) and pulsed dye laser have been shown to alleviate signs and symptoms of REM, these were not used, due to patient photosensitivity.4 Antimalarials, such as hydroxychloroquine, have been shown to be effective and rapid treatments for REM, with significant improvement or complete clearance of skin lesions, however, recurrence is frequent.5
The recurrent erythema had been mistaken for cellulitis and was previously treated with antibiotics oritavancin, ceftaroline fosamil, and doxycycline. Continued recurrence resulted in a dermatology consult. Minocycline was started for its anti-inflammatory properties, along with topical halobetasol QD for two weeks. There was improvement, but the patient continued to flare with tapering. Pimecrolimus was added, but the patient developed flu-like symptoms; therefore it was discontinued. The patient then developed intolerance to minocycline.
Nicotinamide, for its anti-inflammatory properties, and topical halobetasol used only on weekends was found to provide extended remission for the past two years. The patient was recently tapered off of topical halobetasol and has remained symptom-free for the past six months.
This case shows the need to further study of nicotinamide’s anti-inflammatory properties, and its use should be considered for other inflammatory dermatological conditions to avoid steroid and antibiotic overuse.
1. Thareja S, Paghdal K, Lien MH, Fenske NA. Reticular erythematous mucinosis--a review. Int J Dermatol. 2012;51(8):903‐909. 2. Braddock SW, Davis CS, Davis RB. Reticular erythematous mucinosis and thrombocytopenic purpura. Report of a case and review of the world literature, including plaquelike cutaneous mucinosis. J Am Acad Dermatol. 1988;19(5 Pt 1):859‐868.
3. Rongioletti F, Merlo V, Riva S, Cozzani E, Cinotti E, Ghigliotti G, Parodi A, Kanitakis J. Reticular erythematous mucinosis: a review of patients’ characteristics, associated conditions, therapy and outcome in 25 cases. Br J Dermatol. 2013; 169: 1207-1211.
4. Meewes C, Henrich A, Krieg T, Hunzelmann N. Treatment of Reticular Erythematous Mucinosis With UV-A1 Radiation. Arch Dermatol. 2004;140(6):660–662.
5. Kreuter A, Scola N, Tigges C, Altmeyer P, Gambichler T. Clinical Features and Efficacy of Antimalarial Treatment for Reticular Erythematous Mucinosis: A Case Series of 11 Patients. Arch Dermatol. 2011;147(6):710–715.
Ready to Claim Your Credits?
You have attempts to pass this post-test. Take your time and review carefully before submitting.
Good luck!





