An atypical presentation of unilateral, linear, hypertrophic lichen planus in a Patient with HIV
In patients with human immunodeficiency virus (HIV), cutaneous diseases often manifest in atypical or unusual patterns. Here, we report an uncommon presentation of unilateral, hypertrophic lichen planus, in a HIV patient.
Case Report
A 75-year-old Caucasian male was referred to a dermatology practice due to a 4-year history of thick, itchy plaques on his right lower lateral leg which he attributed to his history of diabetes mellitus. He was diagnosed with HIV 20 years prior and has been taking efavirenz, emtricitabine, and tenofovir for years. The patient’s most recent HIV RNA viral load was undetectable and his Cluster of Differentiation (CD) 4 count was 300. The physical examination revealed linear skin-colored to violaceous and verrucous plaques coalescing on the lateral aspect of the right lower extremity, not following Blashko lines. The plaques had an “igneous rock” appearance1 (Figure 1,2). Our differential diagnosis for verrucous lesions in a HIV-positive patient included verruca, molluscum, hypertrophic lichen planus, lichen simplex chronicus, Kaposi sarcoma, squamous cell carcinoma, syphilis, and inflammatory linear verrucous epidermal nevus (ILVEN). A scoop shave biopsy was performed and demonstrated the following histological features: compact hyperkeratosis, epidermal hyperplasia, vertically oriented collagen in the papillary dermis, and civatte bodies near the tips of rete ridges, consistent with hypertrophic lichen planus (Figure 3). He was treated with topical clobetasol ointment twice daily for six weeks which significantly improved his symptoms (Figure 4).

Figure 1: Unilateral, linear, hypertrophic lichen planus on the right lower leg in a HIV patient.

Figure 2: Close up of linear, hypertrophic lichen planus demonstrating an “igneous rock” like appearance.
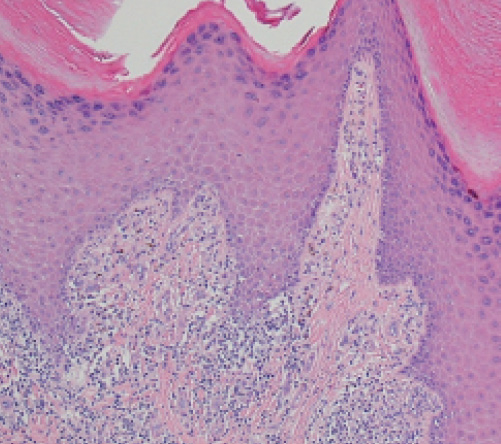
Figure 3: Hematoxylin and Eosin staining of the biopsy of the patient’s right lower leg highlighting the following features: compact hyperkeratosis, epidermal hyperplasia, vertically oriented collagen in the papillary dermis, civatte bodies near the tips of rete ridges, and a lichenoid lymphocytic infiltrate.

Figure 4: Post treatment with clobetasol ointment twice daily for six weeks
Discussion
News and Trends to Note
Does Online Price Transparency Work?
Writing in the October edition of Modern Aesthetics® magazine, Jonathan Kaplan, MD, MPH, founder/CEO of BuildMyBod Health talks about his experience with online price transparency. The full article, available online at ModernAesthetics.com, includes his take on addressing price up-front in order to open up communication about procedures and outcomes. The following is an excerpt:
“The only way to provide the consumer with accurate pricing information without tying up your office staff in tabulating one pricing request after another, is to upload all of your pricing to the cloud. That way, when the con- sumer submits a “wishlist” through a pricing tab on your site (see example on my site here), that pricing is auto- matically tabulated in the cloud and sent to the patient in an email. Again, this level of automaticity is second to none in streamlining front office processes.
“By providing pricing on your website, you’re giving the consumer a level of information they cannot obtain anywhere else. They can’t find your specific pricing for specific services anywhere other than your website. And when you provide that level of personalized information, consumers reward you with their contact info.”
Crowded House
SanovaWorks is raising funds through a crowdfunding campaign to keep Derm In-Review available free-of-charge for dermatology residents and dermatologists undergoing recertification through February 2017. The company has set out to raise $200,000 on GoGetFunding.com to maintain the multi-faceted Board-review program and transition it in Spring 2017 to a web platform that will collect a small fee for non-resident users as well as have the functionality to accept alumni contributions and sponsorship.
Lichen planus subtypes and variants have been previously reported, however, prior to this case report, few cases of lichen planus variants in HIV patients have been described. In immunocompetent hosts, the majority of patients have classic papular lesions, followed by hypertrophic, and actinic lesions. Atrophic, linear, vesiculobullous, annular, lichen planus pigmentosus, lichen planus pigmentosus-inversus, and follicular variants have also been described, but less frequently. One study found that only 3.4 percent of patients with lichen planus had more than one variant of lichen planus simultaneously.2 Hypertrophic lichen planus is commonly described on the anterior legs, ankles, and the interphalangeal joints in a symmetrical distribution.3 Linear lichen planus is an uncommon subtype of classic lichen planus, more commonly seen in the pediatric population (eight percent) than in the adult population (0.2 percent).4,5 Linear lichen planus has been reported to have a Blaschkoian or zosteriform distribution, or caused by a Koebener phenomenon, although the latter is not considered to be a true linear form. The literature does not provide a clear epidemiologic distribution of the linear subtypes.
CALLING ALL DERMATOLOGY RESIDENTS!
The Practical Dermatology® Editorial Board is now accepting submissions for the 2016 and 2017 Resident Resource Center column. The Editorial Board is looking for compelling case studies and original research. Accepted manuscripts will be published in the magazine and online. Please send all submissions to dmann@bmctoday.com for consideration.
There are few case reports of hypertrophic lichen planus in HIV patients per our review of the literature. Prior reports describe the lesions of HIV patients as more widely distributed than lesions in immunocompetent patients.6,7 This was not a feature in our case.
We present this case to illustrate an unusual clinical variant of lichen planus. This case highlights the importance of paying attention to the clinical deviations in cutaneous diseases within the HIV patient population. Also, it is important to diagnose and treat the hypertrophic variant, as there have been some case reports showing malignant transformation in hypertrophic lichen planus.8n
The authors have no conflicts of interest to report with this paper.


Sara M. Wilson is a 4th year medical student at the Uniformed Services University of the Health Sciences (USUHS) in Bethesda, MD.
Tess Pollinger, DO is a 4th year dermatology resident at Walter Reed National Military Medical Center in Bethesda, MD.
George Turiansky, MD is Dermatologist and recently retired United States Army Colonel. He continues to supervise and teach residents at Walter Reed National Military Medical Center as a dermatology consultant and adjunct faculty member. He is also a dermatology professor at USUHS.
1. Welsh JP, Skvarka CB, Allen HB. A novel visual clue for the diagnosis of hypertrophic lichen planus. Arch Dermatol. 2006;142(7):954.
2. Bhattacharya M, Kaur I, Kumar B. Lichen Planus: A clinical and epidemiological study. J Dermatol. 2000;27:576-582.
3. Gorouhi F, Davari P, Fazel N. Cutaneous and mucosal lichen planus: A comprehensive review of clinical subtypes, risk factors, diagnosis, and prognosis. The Scientific World Journal. 2014;2014:742826. doi:10.1155/2014/742826.
4. Sharma R, Maheshwari V. Childhood lichen planus: A report of fifty cases. Pediatr Dermatol. 1999;16(5):345-348.
5. Batra P, Wang N, Kamino H, Possick P. Linear lichen planus. Dermatol Online J. 2008;14(10):16.
6. Emadi SN, Akhavan-Mogaddam J, Yousefi M, Sobhani B, Moshkforoush A, Emadi SE. Extensive hypertrophic lichen planus in an HIV positive patient. Dermatol Online J. 2010;16(6):8.
7. Rippis GE, Becker B, Scott G. Hypertrophic lichen planus in three HIV-positive patients: a histologic and immunological study. J Cutan Pathol. 1994;21(1):52-8.
8. Yesudian P, Rao R. Malignant transformation of hypertrophic lichen planus. Int J Dermatol. 1985;24(3):177-8
Key Dermatology Data
Group physician practices are the new normal, and it seems that dermatologists were ahead of the consolidation curve, according to research in the September 2016 issue of Health Affairs.
The percentage of primary care physicians in the smallest group size declined more than among specialists, and the percentage of primary care physicians in the largest group increased more (4.5 percent, compared to a 1.1 percent among specialists).
There was not nearly as much activity for dermatologists during the period, study author David Muhlestein PhD, JD, Vice President of Research at Leavitt Partners in Salt Lake City, UT, tells Dermwire. “Most dermatologist were already in larger practices, though there was a drop in all practice sizes below 500,” he says. “The takeaway is that larger groups were already the norm for dermatologists, though there is continued movement toward larger groups.”
Ready to Claim Your Credits?
You have attempts to pass this post-test. Take your time and review carefully before submitting.
Good luck!





